Abstract
Health care costs represent a significant percentage of a country’s GDP. Implementing electronic medical records (EMR) systems are a popular solution to reducing costs, with the side benefit of providing better care. Unfortunately, 30% of EMR system implementations fail, often because physicians cannot use the EMRs efficiently. User experience problems, based on our experience at several clinics, are wide-spread among EMRs. These include loss of productivity and steep learning curves.
To help usability professionals contribute to the creation of more usable EMRs, we share our insights and experiences. Essential to understanding EMRs is the physician’s task flow, which we explain in detail. It is also helpful to understand the different work styles of physicians, variations in the pace of work, the use of nurses, the mode and timing of data entry, and variations in needed functionality. These variances in task flow, work styles, and needed functionality lead us to propose solutions to improve the usability of EMRs focusing on: flexible navigation, personalization and customization, accessing multiple patients, delegation of responsibility among medical personnel, and enabling data variations and visualizations.
Practitioner’s Take Away
The following list summarized take-aways that practioners can get from this article:
- Electronic medical records (EMR) have not penetrated the medical field in spite of the benefits that all agree are possible.
- One of the primary reasons for this failure is the lack of usability in the implementation of many systems.
- While incorporating usability in EMR systems presents many unique challenges, these can be addressed and handled by usability professionals.
- These challenges are the result of the difficulty of crafting a system that involves skilled users, complex functionality, and critical tasks.
- Designers of EMR systems should consider the following:
- Employ a flexible navigation scheme to accommodate the variety of specialists, environments, personnel, and individual practices.
- Use appropriate defaults to reduce non-productive work load.
- Enable the rapid switching between patients that is consistent with the way many physicians operate.
- Allow for the delegation of appropriate responsibility to other members of the medical team.
- Provide various methods of data entry that conforms with the way many physicians work.
- Consider innovative visualization, integration, and manipulation techniques to assist in providing superior medical services to patients while minimizing the workload of medical personnel.
Introduction
Medical care worldwide is a costly enterprise. It is most expensive in the U.S., where 16% of gross domestic product (GDP) goes to health care costs. Even the typical Western European country spends 9% of their GDP on health care—a huge amount (OECD, 2006). Paradoxically, the country that spends the most on health care, the U.S., does not have the healthiest population. Most industrialized nations have avoided this dilemma, in part, by implementing electronic medical record (EMR) systems. These systems have other benefits: reducing medical errors, facilitating the electronic transfer of patient records across facilities, and improving the efficiency of clinicians.
However, the story from individual physicians is quite different. They complain of forced changes to established and successful work flows, long training times, and excessive time spent serving the computer rather than providing care to patients. The rush to automate the clinical environment has met significant resistance from clinicians, resulting in some major implementation failures.
Our own experiences with physicians reveal some critical usability aspects of their working environment and the systems they use. We discuss those insights here within the broader context of EMR implementations. Finally, we suggest directions for EMR designs that better accommodate the needs of physicians.
Health Care Problems and EMRs
Medical care can be a costly enterprise for any country. In the U.S., total health care costs stand at $2.2 trillion per year, or about 16% of GDP. This equates to a per capita cost of $7,421 (HHS, 2009). In contrast, most industrialized countries spend less than half that amount, typically less than $3,000 per person per year. The nationalized medical system in the U.K. spends a mere $2,317 per person per year (OECD, 2006).
Countries with wide-spread use of electronic medical records appear to have lower health care costs and better care. Many industrialized countries have improved patient care and controlled costs through the use of EMRs where they are more wide-spread than in the U.S. (Schoen, C., et al., 2006).
A recent survey of 6,000 physicians in seven industrialized countries1 shows that very high percentages of physicians use EMRs, for example, 98% of physicians in the Netherlands and 89% in the U.K. There are also strong correlations between high rates of EMR use and key indicators of clinical care, including access to after-hours care, the use of clinical teams to manage chronically ill patients, and the ability to track medical errors. There is certainly a complex relationship among EMR usage, quality of clinical care, and the implementation of nationalized medicine.
However, there is also a common sense connection between EMR use and better care. If a patient falls ill after-hours, a physician is better able to help if an EMR is available to remotely view the patient’s records. Computerized health records can be easily shared with other providers to facilitate improved care. And computers are infinitely tolerant at cross checking medical interactions to prevent physicians from prescribing medicines with drug-drug reactions or allergic reactions.
Many costly medical errors, including prescription errors, could be eliminated with electronic systems (Eisenberg, 2001). The American Medical Association (AMA, 2006) enumerates eleven benefits of using an EMR system, including potential reduction in medical errors, reduced costs related to chart filing and transcription, and improved communication with other systems (AMA, 2006). There is even a Presidential initiative in the U.S. to speed the implementation of EMRs to “avoid dangerous medical mistakes, reduce costs, and improve care” (Bush, 2006).
Physicians are often enthusiastic about the coming change. In summary, they believe that better information will lead to better treatment. To quote Michael Dotti, M.D., of North Country Family Practice, “An EMR would enable us to keep better track of data. We could treat patients better because information would not fall between the cracks” (Rogoski, 2005, p. 12).
Once implemented, EMRs provide enormous benefits. Time is not lost searching for the patient’s paper chart because all patient information is electronic. Time is also saved when looking through the patient’s chart electronically, a faster process than scanning reams of paper. Also, physician notes and prescriptions are no longer difficult to read because they are typed. Point and click interfaces are a vast improvement over the older text-based 3270 screens. With ready access to the patient’s chart, physicians can provide better care. Costs are also lower to the extent that transcriptionists and chart couriers are eliminated.
EMRs are already arriving at larger clinics and hospitals, and implementation at smaller facilities is inevitable. Unfortunately, all the news is not good.
1. Australia, Canada, Germany, the Netherlands, New Zealand, the United Kingdom, and the United States
Problems with Electronic Medical Records
Finding documented problems with EMRs is a challenge; no one wants to brag about their failures. However, a few prominent failures of medical systems are readily available, namely the physician rejection of the order entry system at Cedars Sinai and the struggles at Kaiser as they tried to implement an EMR system.
Cedars Sinai Medical Center in Los Angeles spent $34 million developing and deploying a physician order entry system for medications, labs, and procedures. Physicians found that it took much, much longer to use the new computer system than did the same ordering with pen and paper. With physicians already working 80 hours per week, there just wasn’t the extra time available. Physicians also found that there were severe limitations on their ability to make medical judgments. To make matters worse, the system failed to recognize words with slight misspellings. And physicians daily faced a flood of excessive electronic reminders, questions, and alerts with the new system. Finally, several hundred physicians refused to use the system, and the administration was forced to cancel the implementation. All this occurred at one of the most wired hospitals in the nation (Connolly, 2005).
Not far away at Oakland-based Kaiser Health Plan, there were many problems with its implementation of the Clinical Information System (CIS), co-developed with IBM. A published study of Kaiser’s experience at their Hawaii clinics revealed numerous problems. However, reduced clinician productivity was one of the key causes. More specifically, clinicians were taking an extra 30 to 75 minutes per day to do their work, because there were too many steps to complete simple tasks, and the system was too cumbersome to adapt to the needs of the clinicians. All these symptoms occurred after an initial learning period (Scott, Rundall, Vogt, & Hsu, 2005).
CIS was ultimately abandoned, and Kaiser is now implementing Epic’s EMR. Unfortunately, there is yet more bad news from Kaiser; the Epic implementation is having difficulties (Rosencrance, 2006). It is possible that Kaiser’s second attempt at an EMR implementation will also join the unfavorable statistics on EMR implementations, where failure rates are around 30% (Connolly, 2005).
What are the underlying causes of these problems? Some authors warn of excessive training costs with EMRs. Also, physicians are reluctant to use a system that takes more time to complete a task. “This is a result of EMRs that have been over-engineered and are not intuitive, forcing physicians to spend more time clicking through screens and menus to get their work done” (Brown, 2005, p. 47). Some clinics report that users often need between six and twelve months before they are comfortable using the new technology. Even after training, physicians are often less productive because the EMR slows them down (Tipirneni, 2006).
The physicians at Cedars Sinai faced excessive time on tasks and an overload of information. Kaiser physicians faced long training times and a loss of productivity. Other users on other EMRs had similar experiences. These problems are hallmarks of systems with usability problems, systems designed without the users at the center of the design process. Our own experience with physicians interacting with EMRs provides insights into the causes of these user challenges.
Problems with EMRs: The Physicians’ Perspective
We have been working with medical systems for several years at Human Factors International (HFI). Two of our prominent clients are the Indian Health Service (IHS), a division of Health and Human Services within the U.S. Government, and the Mayo Clinic. IHS and the Indian Tribes provide medical care to 1.9 million American Indians and Alaska Natives through a network of 45 hospitals and 288 health centers. The Mayo Clinic is a world-renowned medical practice based in Rochester, MN.
Our observations on EMRs are based on visits to several IHS facilities with dozens of health care providers using a single EMR system that has been locally customized. We also base our insights on an extensive cross-facility usability review for Mayo Clinic. For this review, we visited four different clinics in Rochester, Boston, Jacksonville, and Madison and observed approximately 20 physicians at work with four different EMRs.
Overall, our observations support insights from the literature. Physicians, indeed, find that EMRs take a long time to learn and often make them less productive. Physicians experience specific usability problems when working with EMRs that cause long training times and loss of productivity.
Long Training Times
EMRs provide an enormous range of functionality. This complexity can be bewildering for beginning users, and it simply takes time for them to understand what can be done and how to do it. This is typically a problem with the navigational structure of the EMR system. A typical EMR system contains hundreds and hundreds of screens that need to be accessed through the system’s navigational scheme using tabs, buttons, and hyperlinks. Learning the right paths takes time.
Loss of Productivity
Even after a physician has learned to use the EMR, it often causes him or her to be less productive. The causes are many:
- Difficulty finding important information, e.g., Which note is the last full note? When was the patient’s last mammogram? Does the patient need a tetanus shot?
- Typing the note is slower than writing it out.
- Some tasks are tedious to complete with the EMR, e.g., reordering chronic medications.
- The system response time can be long.
- Changing exam rooms requires logging off one workstation and enduring a lengthy login to a new one.
- Lack of integration places information needed for one task on multiple screens, e.g., reviewing lab results as affected by a change in medications.
- Searching for a procedure or diagnosis can produce useless results. Physicians speak one language, but the procedures and diagnoses are sometimes based on a different set of codes.
- Some screens contain information that is not needed, but missing information that is.
- Some screens are densely packed with information, making information hard to find.
This is only a partial list, and the list for each EMR system is different.
The Fundamental Problem: Skilled Users, Complex Tasks, and Complex Functionality
Fundamentally, usability problems arise in EMRs because of the interaction of three very complex components: physicians, their tasks, and the EMR. Physicians are highly trained professionals with very large knowledge bases and deep problem solving skills. In addition, physicians specialize in one of dozens of specialties. The tasks they complete, diagnosing and treating illnesses, are very complex and high risk. Finally, to support physicians as they complete their tasks, they need a very complex but efficient information system. Making complex systems usable is extremely difficult. It is no surprise that most EMRs struggle with usability.
Our focus in this paper is on the users’ tasks. We certainly cannot cover all aspects of medicine known to physicians. Nor can we dive into all the usability problems of EMRs. Instead, we will focus on the tasks that physicians complete in the course of a patient encounter and highlight the corresponding usability problems that arise from variances in the way physicians work.
Variances in User Tasks
Overall there is enormous variability in the way that physicians work. Some examples include variations in the pace of work, the use of nurses, mode and timing of data entry, timing of patient load, task flow issues, and variations in needed functionality. Each of these deserves a brief explanation along with the corresponding usability issues that arise.
Pace of Work
The pace of work across physicians is highly variable. Some physicians see one patient per hour; some see four patients per hour. Logging in and out of a workstation as the physician rapidly changes exam rooms can be both annoying and unproductive. It gets worse for the physician if he or she is seeing more than one patient at a time, as is typical for many specialists.
Delegation of Work
The delegation of work varies across physicians. Some physicians do everything from taking vitals to ordering tests to reviewing systems. Others rely on assistants or nursing staff to complete work, either directly (e.g., instructing the nurse to order an MR scan of the patient’s sinuses) or indirectly (e.g., nurses often have standing orders to administer routine tests and immunizations). Unfortunately, one system we observed requires that the nurses log into the EMR as themselves but order labs and procedures via proxy. This is a tricky process that will send the lab results and procedure results not to the ordering nurse but to the physician who needs to see them. If it is not done correctly, the physician will never see the results.
Data Entry
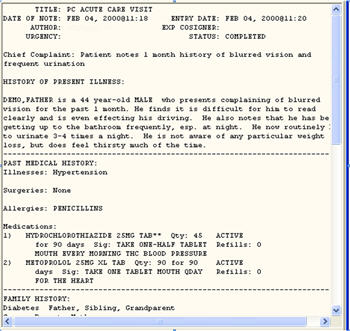
Getting data into the system can be done in different ways, and each provider has his or her preferences. (See Figure 1 for a sample note.) Younger physicians tend to be touch typists, while older physicians tend to prefer dictation. However, many physicians still prefer to write, and this can be done with a tablet. Finally, some physicians prefer combinations, e.g., importing boilerplate data, like medications and labs, while typing in their plans. One major EMR system we saw did not support dictation, forcing non-typists to hunt and peck. In another case where dictation was available, the department head mandated that all physicians type in their notes so that they would be immediately available. (Dictation typically requires a 24 hour turnaround.) This was a significant burden to non-typists.
Figure 1. Sample note
Timing of Data Entry
The timing of data entry can be highly variable. Some physicians enter the note with the patient present, while others wait until the patient has left the exam room. Those with busy schedules tend to wait until the end of the day to enter their notes for all patients. Waiting until the end of the day to enter notes is potentially risky, as it relies on faulty human memory to reconstruct what occurred hours earlier.
Task Flow Variability
The physician’s task flow can be highly variable and frequently interrupted. One physician may always review the patient’s chart, then interact with the patient, then order labs, medications, and consultations with specialists, before composing the note and recording billing. Another physician may first interact with the patient, then order labs, then review the patient’s chart, then order medications, and finally wait until the end of the day before composing the note and recording billing. (See Figure 2.) Both physicians, though, are constantly interrupted by their beepers, their phones, and the paging system. When this happens, they often lose track of where they are in their task flow because the EMR interface does not change to show which subtasks have been started or completed. This forces the physician to lose time by reviewing current work or face potential safety issues from incomplete work. (See Figure 3 for sample navigation structure from an EMR.)
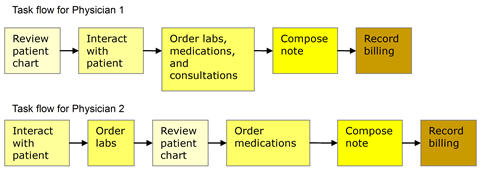
Figure 2. Two different task flows for the same task
Figure 3. EMR navigation with no feedback on completed steps
Also, many of the EMR systems we saw did not support rapid switching from one patient to another and back again. This situation is surprisingly typical where physicians are interrupted at least once per hour by pages to attend to another patient’s record. Switching between patients then becomes a frequent but time-consuming process.
Need for Different Functionality
Not surprisingly, different specialties need different functionalities. Obstetricians need a special set of vitals on the developing child. Ophthalmologists need to record drawings of eyes. Radiologists work with digitized images. Each specialty typically needs a specialized interface to support their unique needs. Unfortunately, not all EMRs provide this level of customization. Most systems we saw rely on a text-centric interface for recording physicians’ notes; no drawings are possible. Another system at a remote clinic expected the local tech staff to customize screens for each of the specialties. However, the differences between specialists do not end with functionality.
Different Perspectives on Health
Different specialists have different perspectives on patient health. Certainly all physicians wish to “heal the lame.” Orthopedists fix broken bones and surgeons repair damaged organs. However, in family medicine, and often in internal medicine, they are more focused on prevention, particularly when seeing a patient for a regular check-up. Getting a timely flu shot, getting regular mammograms, and controlling cholesterol levels can have enormous long-term health benefits. As a result, different physicians often need to see different information about the same patient. Unfortunately, the interfaces we saw in popular EMRs did not take these differences into account. In general, prevention-oriented family doctors saw the same user interface as orthopedists.
All these task differences—in pace of work, in delegation, in data entry, in functionality, and in perspective—contribute to the challenge of designing a usable EMR. However, there are yet more challenges that usability specialists face.
Challenges to Studying Usability in Clinics and Hospitals
Usability work with EMRs is not straightforward. Usability professionals, in our experience, face significant challenges in clinical environments when tasked with making an EMR more usable. Clinicians use foreign terminology; clinicians have very broad and deep knowledge; physicians have enormous power (political as well as life-and-death) in clinical settings; and privacy as well as limited access to busy physicians can keep usability professionals from observing physicians at work.
One challenge to understanding users and their tasks is the depth and breadth of user knowledge. All physicians have broad knowledge of human health, medications, and medical procedures. Typically, though, each physician also has deep knowledge in a specialty area, such as internal medicine, pediatrics, OB/GYN, family medicine, ENT, oncology, radiology, and pharmacology. You can imagine observing three different specialists before lunch where each one discusses a different organ system, orders different tests, and prescribes different medications. To make life more challenging, different specialists also tend to use different aspects of the EMR in their work.
A usability colleague of mine once said, “Ignore the differences between users. Focus on what most users do most of the time.” Unfortunately, this recommendation will probably not work in the world of medicine, where a few physicians wield enormous power over the operation of the clinic. Also, physicians in different specialties need specialized user interfaces to be productive.
Medical systems use a myriad of codes to describe the diagnoses made by the physician and the procedures that physicians order. If someone has diabetes, there is not just one code to describe it but dozens. For example, the ICD-9 category for diabetes mellitus is 250, but 250.62 is the specific code for type II diabetes mellitus with neurological manifestations. And those last two digits, .62, are required to describe an adult with diabetes on insulin who has nerve damage. Similarly, there are hundreds of codes for the procedures that a physician can order. Measure blood oxygen level is 94761, while a TB intradermal test is 86580.
Beyond codes are the hundreds of commonly prescribed medications. Some of the most commonly prescribed medications are Lipitor (cholesterol), Prevacid (acid reflux), Atenolol (beta blocker for high blood pressure), Prozac (antidepressant), and Zoloft (antidepressant). Then there are pain relievers, tranquilizers, allergy medicines, antibiotics, medicines for blood pressure, sleeping pills, and stomach remedies. Each comes in different dosages taken with different frequencies at different times of the day. And they often interact with each other and with peoples’ allergies. The complexity of drugs is truly bewildering.
Beyond the lingo of medicine are the settings in which medicine is practiced. Most of us have been in an exam room at a clinic. How many of us have been in an exam room with a physician and a complete stranger? Almost none of us. Patients often want privacy, and there are privacy regulations that limit access to personal medical information. Also, physicians are very busy and sometimes reluctant to be observed while practicing medicine.
Understanding Physicians at Work: Insights into Users, User Tasks, Environment, and Medical Information
Understanding health care providers at work is clearly a daunting challenge for most usability professionals with limited medical knowledge. Your own individual experience with doctors and nurses gives us some limited understanding of what they really do. A visit to the local clinic with a sore throat will serve as a convenient baseline.
Visiting the Clinic
If you wake up tomorrow morning with a sore throat and a fever, you might decide to see a doctor. Here are typical steps you might follow:
- Call for appointment. Good news. They can fit you in at 3 p.m.
- You appear at the clinic at 3 p.m. and start filling out paperwork: health insurance information, medical history including surgeries, family history of ailments, and current medications. You also watch TV and browse the magazines.
- The nurse sees you at 3:30 p.m. and takes your temperature, blood pressure, heart rate, and measures your height and weight. He or she also asks what’s wrong and how long you’ve had symptoms.
- The doctor appears at 3:40 p.m. He or she looks at your throat, up your nose, and in your ears. “The flu is going around, and you’ve probably got it. I’m going to prescribe a new anti-flu medicine, Tamiflu. Which pharmacy do you use?”
- On the way out the door, you stop at the receptionist to write a check for the co-pay on your insurance.
Let’s look at this from the doctor’s perspective. Specifically, Figure 4 shows a task analysis for a doctor of internal medicine who is seeing a patient in an outpatient setting. During the clinic visit, you actually experienced three of the 16 subtasks, circled in orange in Figure 4, that the provider typically completes. You also experienced several administrative subtasks not related to medical care, i.e., filling out forms and paying for the visit, along with many minutes of reading old magazines, watching TV, and browsing colorful brochures on osteoporosis and circumcision.
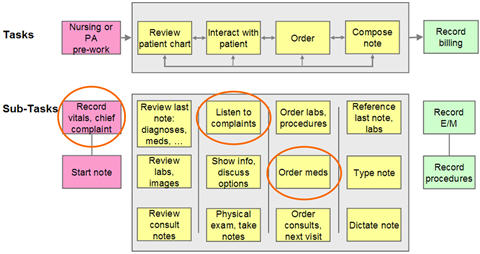
Figure 4. Task Analysis for a doctor of internal medicine
Task Analysis
Understanding medical systems starts with understanding the tasks that providers typically complete, as shown in Figure 4. At the highest level, there are the following six major tasks that providers complete for each patient encounter:
- Nursing or physicians assistant (PA) pre-work
- Review patient chart
- Interact with patient
- Order labs, procedures, medications, and consultations with specialists
- Compose the note
- Record billing
Tasks two through five can be done in almost any order, and each provider typically has his or her own favorite order. I observed an oncologist start with step 3 (interact with patient), go to step 2 (review patient chart), and finish with step 4 (order labs, procedures, and medications). Naturally, if the patient had questions, he would jump back to step 3 and could go anywhere from there, depending on the patient interaction, what appeared in the patient’s chart, and what problem-solving approach he pursued. At the end of the day he composed the note.
The patient encounter starts when a nurse first sees the patient in the exam room. Here the nurse typically measures and records the patient’s vitals, including height, weight, heart rate, and blood pressure. The nurse also asks, “So, what brings you into the clinic today?” Whatever the patient says next will be translated into the chief complaint and is typically recorded in the system.
The physician often reviews the patient’s chart next for two reasons. First, the patient may be here as a follow-up to a prior visit, which is documented in the chart. Second, the patient’s current health problem is typically related to prior health problems, e.g., diabetics typically have related health problems including retinopathy, neuropathy, and renal failure.
Interacting with the patient will inform the physician’s next steps. It is part examination and part conversation. The examination involves a physical examination of the patient, sometimes reviewing all major systems, i.e., circulatory, skeletal, gastrointestinal, etc. The discussion involves understanding the patient’s current problems and discussing alternative treatments.
Ordering is an internal process whereby the physician orders other parts of the clinic to complete work on or for the patient. For example, the physician can order blood tests (labs), an MR scan (procedure), a prescription for penicillin (medications), a consultation with a specialist in ENT (consult), and a follow-up visit.
Each time a physician meets with a patient, the physician must record what happened in a note. Notes come in different sizes, but essentially it is a written record of the vitals, the chief complaint, the current medications, any lab results, the results of the examination, the diagnosis, and the orders placed for labs, procedures, medications, etc. Composing the note often takes more time with a computerized system than with the old paper-based system.
Finally, the physician must record the work done so that the clinic can get paid. This involves identifying the Evaluation and Management (E/M) code and recording any procedures completed. Billing for services is an enormously complicated process and beyond our scope.
This understanding of the tasks and task flows completed by physicians was essential to our analysis of EMR usability. It is also central to good user-centered design. With this solid understanding of users’ tasks, we can now revisit the challenges that physicians face with EMRs to look for ways to improve their EMR experiences.
Directions for Future Medical Systems
Based upon our discussions and observations with the various medical personnel, we are proposing several design directions that future medical systems should consider. These design directions are not necessarily specific to medical systems but are crucial to the success of future systems.
Flexible Navigation Scheme
As we noticed, the road to effective patient care can take many paths, not only by the variety of medical personnel but also within the physician category. It is therefore important to create a flexible navigation scheme that can be tailored to a particular medical environment and even customized by individual physicians. The navigation schemes must reflect the mental model of the medical professional and not those of the designer or even the medical administration.
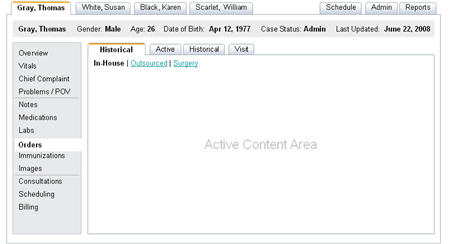
Figure 5. Possible navigation model with multiple levels
One scheme (Figure 5) employs a top level patient tab, a left navigation categorization, a set of relevant sub tabs, and even a further breakdown in the active content area. This model provides rapid access to many patient areas with a minimum number of clicks. The listed items can be tailored to a particular medical system or practice, or even customized to a specific physician. It must reflect the users mental model and in particular their terminology.
Accommodate Specialists
Physicians with different specialties need different functionality and different information. Physicians typically have different specializations: internal medicine, ophthalmology, ENT, radiology, surgery, etc. They need different summary information for each patient and different functionality. An ophthalmologist would see summary information about each patient’s visual system and be able to sketch a patient’s retina, while an obstetrician would see summary information on the developing fetus and be able to record information on it. Even with a customized user interface, there are individual differences within a specialty. This implies that they need an interface customized for their specialty. However, many individuals will want to personalize that interface for their individual needs to better match their individual task flows and data entry preferences.
Use of Defaults
The pace of work varies greatly across physicians and clinics, from one patient per hour to six or more patients per hour. In the latter situation, typically where acute illnesses like flu and colds are being treated, there is no extra time to thoroughly document each patient visit. However, there are also a small set of problems seen in such clinics. As a result, the interface can dramatically simplify handling common problems, e.g., sore throat. Rather than separately entering the chief complaint, ordering labs, prescribing meds, and typing notes, the interface can record defaults for labs, meds, and notes once the physician selects sore throat as the chief complaint. Obviously, these defaults can be changed if the patient’s situation demands it.
There is of course a potential problem with the extensive use of defaults. If the default entry is not verified by a physician, incorrect data may be entered in the patient’s record simply because it was included in the default package. This can be problematic, for example, where medications are involved. A thorough analysis must be performed to determine the appropriateness of defaults. It must however be remembered that repetitious entry becomes automatic, even annoying, and essentially serves as a de facto default.
Accessing Multiple Patients
The pace of work also varies in the number of patients being treated at any one time. Physicians who treat multiple patients at any one time by using several exam rooms are often penalized by EMR systems that require them to log out when leaving one room and log in when entering another. The user interface should also support rapidly switching between patients, because physicians are often interrupted during an exam by a high priority call about another patient. The first level of tabs in Figure 5 shows a possible multi-patient navigation scheme. In addition, a usable EMR should allow the physician to inherit the login used by the nurse who took the vitals and recorded the patient’s chief complaint to reduce the initial login time. Finally, implementation teams should consider portable tablet PCs so that the physician is always connected and never has to log out or back in.
Appropriate Delegation of Responsibilities
Physicians vary in how they delegate responsibilities to nurses or assistants. In the same way that the physician can inherit the login used by the nurse, the nurse should be able to complete the administrative aspects of the visit, e.g., administer and record inoculations. Parallel work on one patient by both the physician and the nurse requires that the EMR allow simultaneous access to the same patient record, even though many database systems limit simultaneous access. Also, results from the labs ordered by the nurse should go to the physician, not necessarily the nurse. The UI needs to support this redirection quickly and easily, with clear and appropriate redirection status displayed on relevant screens.
Data Entry Variations
Different physicians prefer different methods for entering their notes, primarily because of productivity issues. Those with strong typing skills will prefer to type when entering notes from patient visits. Those comfortable with dictation will prefer to dictate their notes. Others will want to write their notes onto a tablet interface. As well, a tablet interface will also be important for sketching pictures of eyes, hands, and other anatomic characteristics.
However, the method employed for entry affects successful searches for relevant patient information. If physicians enter data as free-form text, then subsequent physicians will struggle to search it for specific information, e.g., “When was this patient’s last mammogram?” The answer may be buried in one of dozens of separate notes. There are no easy answers to mitigate this complexity.
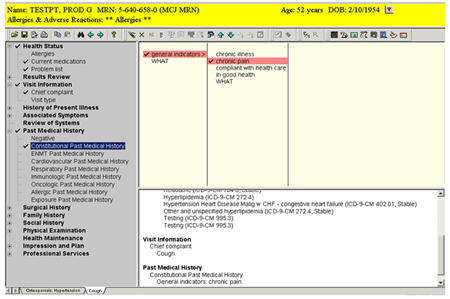
Figure 6. Example structured editor for note entry
One approach would be to encourage physicians to use structured text (Figure 6). While this approach sounds promising, the usability of the templates must be thoroughly user-tested to ensure that it meets the needs of both data entry and retrieval. As more and more physicians become computer savvy, this problem may diminish.
Data Visualization
Finally, physicians are very intelligent, highly trained individuals solving problems with a very complex system—the human physiology. The interrelations and dependencies with the human body are immense. As EMRs enable physicians to access ever greater amounts of information, they will need to see that information displayed in formats that can be integrated and manipulated. This may involve the use of multiple monitors and sophisticated software. Hospitals and clinics promise to be a fertile ground for data visualization software and for the manufacturers of display hardware.
Conclusions
Obvious problems with EMRs, such as loss of productivity and long training times, have deeper causes. These stem from the complex interaction of highly skilled physicians trying to complete complex tasks in a challenging work environment with a complex and not always usable medical information system. Yet, by applying user-centered design in this complex environment, usability professionals can contribute significantly to improving EMR usability. Greater productivity and lower costs with better health care may yet be our destiny.
References
American Medical Association (AMA), (2006 October 24). Benefits of an EMR. Retrieved on May 2007 from www.ama-assn.org.
Brown, N. (2005, May). Driving EMR Adoption: Making EMRs a Sustainable, Profitable Investment. Health Management Technology, 25(5), 47-48. Retrieved on May 2007 from www.healthmgttech.com.
Bush, G.W. (January 20, 2004). State of the Union Address.
Connolly, C. (2005, March 21). Cedars-Sinai Doctors Cling to Pen and Paper. The Washington Post, p. A01. Retrieved on May 2007 from
http://www.washingtonpost.com/wp-dyn/articles/A52384-2005Mar20.html.
Eisenberg, D. (2001, April 23). To the Rescue!, Time, 157(16), 34-36.
Health and Human Services, Centers for Medicare and Medicaid Services (2009). National Health Expenditures 2007 Highlights, Retrieved on January 2009 from http://www.cms.hhs.gov/NationalHealthExpendData/downloads/highlights.pdf.
Organisation for Economic Co-operation and Development (2006, October 10). Health Data 2006, subscription database, Retrieved on May 2007 from http://www.oecd.org/health/healthdata.
Rogoski, R. (2005, May). Look Before You Leap, Health Management Technology, 26(5), 10-15 Retrieved on May 2007 from www.healthmgttech.com.
Rosencrance, L. (2006 November 16). Problems abound for Kaiser e-health records management system, Computerworld, 40(46), 1-3 Retrieved on May 2007 from http://www.computerworld.com/action/article.do?command=viewArticleBasic&articleId=
9005004.
Saporito, B. (2005, June 20). The e-Health Revolution, Time, 165(26), 55-57.
Schoen, C., Osborn, R., Huynk, P. T., Doty, M., Peugh, J. & Zapert, K. (2006). On the Front Lines of Care: Primary Care Doctors’ Office Systems, Experiences, and Views in Seven Countries, Health Affairs, 25, pp. 555-571.
Scott, J. T., Rundall, T. G., Vogt, T. M., Hsu, J. (2005 November 3). Kaiser Permanente’s experience of implementing an electronic medical record: a qualitative study, British Medical Journal, 331:1313-6, Retrieved on May 2007 from http://www.bmj.com/cgi/content/abstract/331/7528/1313.
Tipirneni, K. (2006). The Problem with EMRs, Stryker Imaging, Retrieved on May 2007 from www.stryker.com/imaging.